Beyond Baby Books - MyHealthyPregnancy App Guides What to Expect When You’re Expecting
By: Gina Edwards
The pregnancy journey comes with its fair share of questions.
Is bleeding normal? Why are my moods changing? Are vaccines safe to receive while pregnant?
Searching such health questions on the internet rarely leads to quality answers, as anyone who has gone down a WebMD rabbit hole knows. But what other options do pregnant people seeking quick answers have in between appointments?
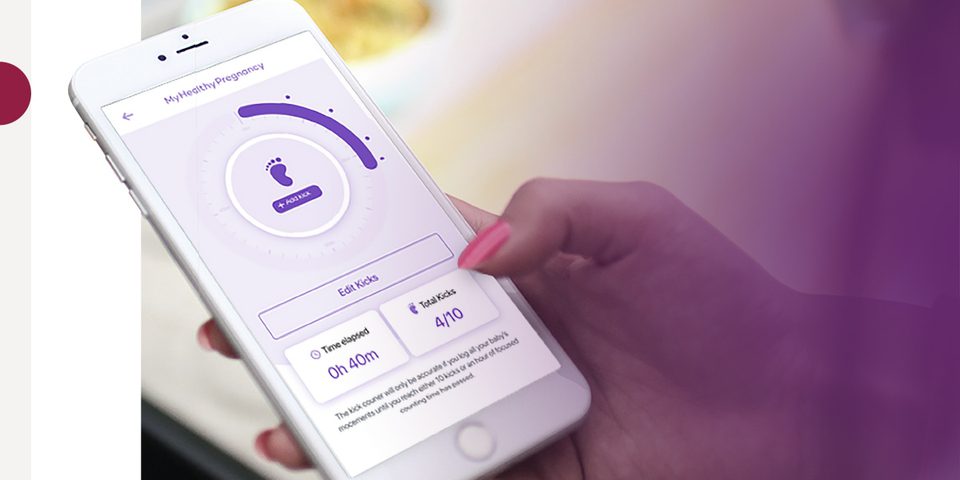
Enter, MyHealthyPregnancy (MHP): an educational app addressing risk factors contributing to preterm birth, or births prior to 37 weeks of gestation. By digitally communicating doctor approved information on-demand to pregnant patients, developers of the MHP app aim to address disparities — as preterm birth is experienced by women of color, particularly Black women, at disproportionately high rates.
“We really wanted to prioritize creating something that will be cognizant of the needs of people who have been historically denied access to resources and access to high-quality health care,” explains Dr. Tamar Krishnamurti, an investigator at Magee-Womens Research Institute (MWRI) and assistant professor of medicine and clinical and translational science at the University of Pittsburgh. “We also wanted to make sure that at no point our tool perpetuated inequities in health or health care delivery.”
To accomplish these goals, a collaborative team across MWRI, the University of Pittsburgh, and Carnegie Mellon University (CMU) focused their work on beginning with in-depth learning from community members’ lived experiences. Along with Dr. Krishnamurti, the founding members of the group included Dr. Alexander Davis, a former CMU faculty member in engineering and public policy, and Dr. Hyagriv Simhan, a practicing maternal fetal medicine physician, and an experienced clinical and translational perinatal researcher.
Formative Research in the Community
Hazelwood is a 1.5-square-mile neighborhood located 2.3 miles from UPMC Magee-Womens Hospital. In 2017, the MHP team partnered with the Hazelwood community organization, Center of Life, to interview and gather perspectives from local individuals.
“We did a lot of our formative research talking with pregnant people in the Hazelwood community — understanding what their needs were, their barriers to accessing care, and their own mental models of pregnancy risk,” Dr. Krishnamurti says.
The research team asked respondents open-ended questions about what is perceived as routine or risky in pregnancy, from things like spotting or bleeding to increases in anxiety. The data gathered from this stage laid the foundation for how MHP would deliver communication to patients.
“When we were conceiving MyHealthyPregnancy, we initially planned to create a suite of written communications just to try and bridge gaps in patients’ knowledge about risks that were related to preterm birth,” says Dr. Krishnamurti. “But as we were thinking through that process and bringing our different areas of expertise together, we realized that smartphones were ubiquitous, especially among people of reproductive age, and offered a more dynamic way to tailor information.”
Dr. Davis used his expertise in machine learning and applied statistics to develop and build the tool using predictive models for certain pregnancy risks. In other words, MHP features sets of preprogrammed questions to help patients and their providers understand if they are on a particular risk trajectory.
“The ability to make digital communications dynamic was really appealing as we got into thinking about the best ways to create communications,” Dr. Krishnamurti says. “We decided that we would take the work that we were doing and implement it into a smartphone app that could combine our expertise in medicine, machine learning, and behavioral science and build something that could better identify and communicate to people about pregnancy-related risks.”
MyHealthyPregnancy in Practice
To develop and commercialize the MHP app, the founding team members formed Naima Health, a company that “develops health tools using behavioral decision science and machine learning to engage patients in their clinical care.”
In early 2020, the MHP app launched and became integrated into clinical care processes.
Once a patient confirms their pregnancy at a UPMC facility, they receive a text message inviting them to use MHP as a supportive tool for their pregnancy journey. A physician portal also allows providers to navigate through their patient’s electronic health chart and see select information shared through the app.
Since its rollout, providers have prescribed the MHP app to more than 15,000 people.
“As a patient, you enter information into the app throughout your pregnancy — things like your symptoms or your mood or challenges that you may be facing in your life. The app will then provide tailored feedback on that pregnancy and connection to the vetted resources both inside and outside the health care system,” says Dr. Krishnamurti.
The goal is twofold: identify pregnancy risk factors earlier than routine care can and offer reassurance to people when things are going perfectly fine. MHP supports both veteran and first-time pregnancies but is particularly helpful to those whom the pregnancy journey is new for.
“In a first-time pregnancy you’re not quite sure how to distinguish between what is the normal course of pregnancy and what feels like a very big change in your in your body,” Dr. Krishnamurti says. “One of the things that we heard frequently during our formative qualitative work and in building this tool is that — as a pregnant person — you can sometimes get totally overwhelmed with the amount of information.”
Dr. Krishnamurti explains that when well-intentioned patients try to stay informed by googling risks and what could be going wrong, the information search can worsen their anxiety. That is why the team wanted to build the app as a reliable source of information that also would not leave patients uncertain.
“We don’t ask about or push information back to anybody about a risk unless it is actionable information. That was philosophically really important to us,” she says. “We wanted it to be a support tool and not an additional source of worry.”
Early Results: Closing Care Gaps, COVID Guidance, Spanish Version
With nearly three years of the app being used by the public, the team already has early data, wins, and updates under their belt.
Of those prescribed MHP, a little over half are using it. There is a higher use of MHP among those with a risky medical history or who are experiencing risks, as well as those with social determinants of health challenges. Over time, those with smooth pregnancies tend to use the tool less frequently.
“That [data] tells us we’re reaching the people that have the greatest need and that patients who are experiencing fewer risks are appropriately realizing that they need less support and using it less over time,” Dr. Krishnamurti says.
Launching and testing the tool also allowed the team to help close gaps in care, particularly with patients facing mental health emergencies.
“If someone shares something like thoughts of self-harm into the tool, then we can send that information directly to a nursing team who then can do an outreach to the patient,” Dr. Krishnamurti says.
Since MHP launched right before the COVID-19 pandemic, the team incorporated COVID symptom triaging and appropriate avenues for care at a time when there was little information about COVID and pregnancy. Additionally, the tool has helped identify gaps in patient-provider communications, especially for particular risk factors like preeclampsia.
“We found that patients who are at risk for developing preeclampsia won’t always be aware of their doctor’s recommendations to take low-dose aspirin, which can actually decrease preeclampsia risk,” she explains. “So, we’ve been able to use that information that we’ve collected from the app to give feedback to the health care system about how to improve their care processes.”
Thanks to CDC funding, the team also created a Spanish-language version of MHP with information tailored for emerging Latino communities.
Evolving MHP Toward the Future
As thousands use the app, the MHP team continues to gather data to better understand patients’ symptoms and experiences around pregnancy risks like hypertension or depression.
“UPMC has been an amazing system to start out in,” Dr. Krishnamurti says. “It’s an integrated finance and delivery system, so there are many different bodies of the organization working together. To be able to build a tool into that kind of system has been challenging but has also allowed us to evaluate it rigorously.”
Dr. Krishnamurti credits piloting the app at UPMC for the ability to test and optimize MHP, which has set the stage for its future. “We’ve been fairly scrappy in building and launching something with a small team and limited resources,” Dr. Krishnamurti says. “But we’ve also been thinking about ‘How do we scale?’ and ‘How do we grow?’ and ‘How do we continue to reach patient populations that would be best served by this?’”
Even as the group looks to expand its work, they are committed to maintaining partnerships with physicians and new parents so that the app can evolve and grow along with the people being served. For Dr. Krishnamurti, the ultimate goal is simple: to support patients. “If we’re able to use tools like MyHealthyPregnancy to more effectively direct resources to those patients that need them, I think that that’s the dream outcome.”