MWRI Faculty Members Receive Over $18 Million in Latest Round of NIH Grants

Dec 3, 2024
Areas of Research Include Cardiovascular Health, Infertility, Ovarian Cancer, Pelvic Floor Disorders, Preterm Birth, and Addiction Medicine
By: Gina Edwards
Contact: Joan McSorley • mcsorleyj3@mwri.magee.edu
FOR IMMEDIATE RELEASE
Investigators at Magee-Womens Research Institute have received over $18 million in grant funding from the National Institutes of Health, in areas including cardiovascular health, infertility, ovarian cancer, pelvic floor disorders, preterm birth, and addiction medicine.

Dr. Kyle Orwig received a 4-year $6,583,000 P50 competitive renewal grant from the NIH, titled “Genetics of Male Infertility: Accelerating the pace of discovery.”
About 50% of patients who seek infertility care receive a heartbreaking response: their infertility is unexplained. A genetic cause is suspected in many of those cases, but we don’t yet know the genes. “I meet patients every single day that have a fertility problem that doesn't have a solution. And as a researcher, that's the kind of thing you bring back to the laboratory,” says Dr. Kyle Orwig, principal investigator.
Context: Azoospermia, a condition where semen contains no sperm, affects 1% of men globally, which translates to about 645,000 individuals between the ages of 20 and 50 in the United States. Dr. Orwig adds that this is the “worst kind of diagnosis” because it currently means there is no option to have a biologically related child.
Project Aim: The team aspires to generate improved knowledge about the genetic basis of infertility to aid in the counseling of infertile couples, justify the development of diagnostic screenings, and lead to patient-specific treatment options.
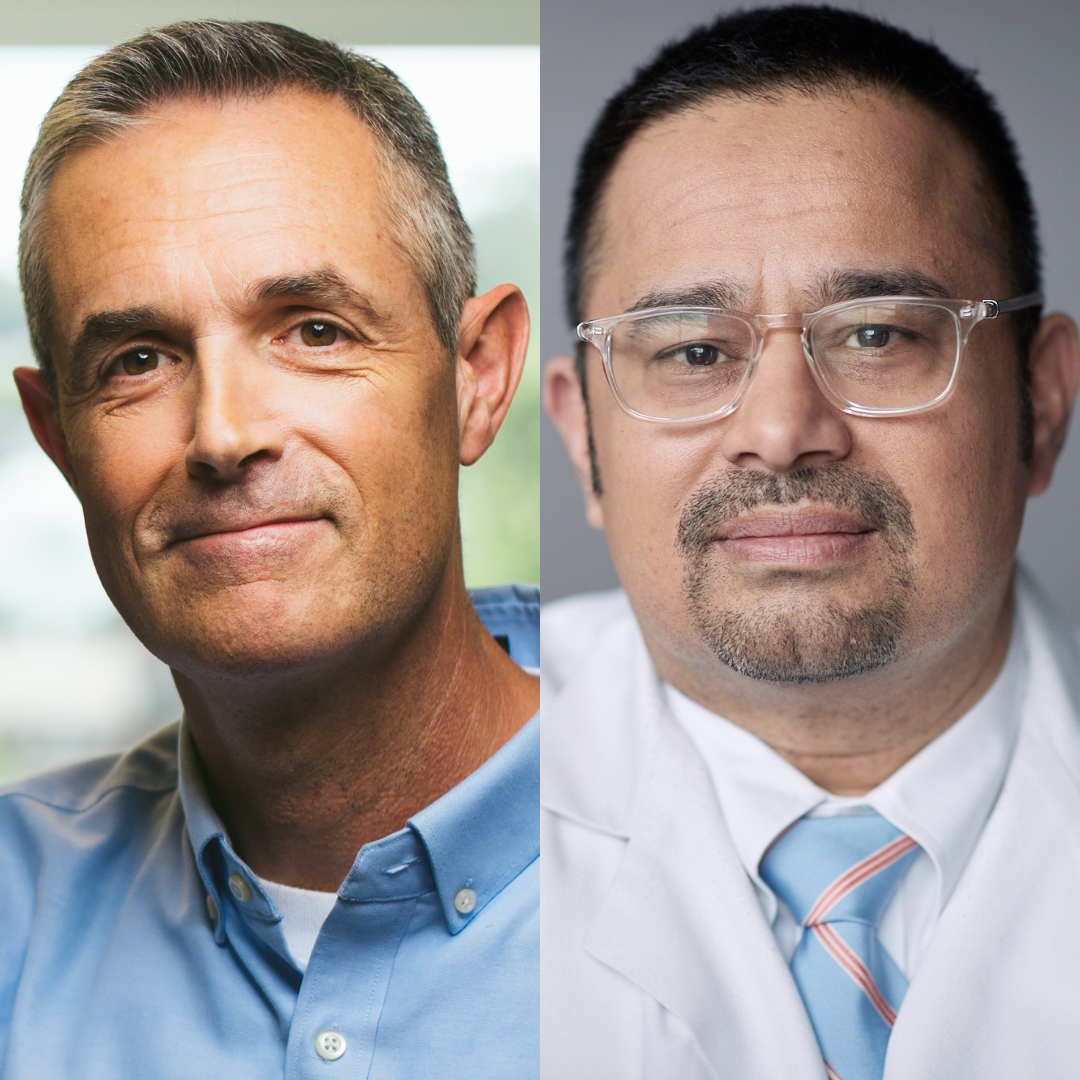
Drs. Dave Peters and Hy Simhan received a 5-year $3,437,000 R01 grant from the NIH, titled “Development of Non-invasive Liquid Biopsy Screening Tool for Preterm Birth Causes and Consequences.”
Context: Preterm birth (PTB) is the second leading cause of death in children under the age of 5 years. In 2010, more than one million infants born preterm (less than 37 weeks of gestation) died worldwide.
Project Aim: This research aims to improve our understanding of the biology of PTB and lead to the development of new diagnostic or screening tools to identify women at high risk who are most critically in need of intervention.
“We are grateful to NICHD for their support of our work to deepen our understanding of the biology of preterm birth, and, most importantly, identify prediction and prevention strategies that integrate effectively into modern prenatal care,” says Dr. Simhan.

Dr. Janet Catov received a 5-year $3,912,000 grant from the NIH, titled “Expanding the Family Check-Up in Early Childhood to Promote Cardiovascular Health of Mothers and Young Children (ENRICH).”
Context: Cardiovascular disease (CVD) is the leading cause of mortality in the U.S., with significant disparities based on race, socioeconomic status, and geography. Early lifestyle interventions can reduce CVD risk. American Heart Association’s “Life’s Essential 8” lists diet, physical activity, sleep, smoking, cholesterol, weight, blood pressure, and glucose as key to a life course approach to cardiovascular health (CVH). Home visiting programs, active nationwide, are uniquely positioned to address CVH in prenatal and postpartum individuals and their children through sustained interactions with families in home settings, especially in underserved communities.
Project Aim: The ENRICH trial aims to evaluate the effectiveness of integrating CVH-promoting interventions into evidence-based home visiting programs. The study will assess improvements in maternal CVH behaviors, such as diet, activity levels, and BMI, at 12 and 24 months postpartum and in children's BMI trajectories and CVH behaviors at 24 months. It also examines subgroup differences and implementation feasibility to inform broader adoption.

Dr. Pam Moalli received a 4-year $2,258,299 grant from the NIH, titled “Pubovisceral muscle enthesis injury: a bioinspired approach to repair.”
Context: Each year, 20% of women who give birth vaginally suffer injuries to the pubovisceral muscle, which significantly increases their risk of pelvic organ prolapse (POP) later in life. POP is a chronic condition affecting millions of women, with 12.6% of U.S. women requiring major surgery for POP by age 80, resulting in over $10 billion in annual healthcare costs. These injuries often go undiagnosed during childbirth, and there is currently no effective treatment to repair the damage, which undermines the success of existing POP surgeries.
Project Aim: This project aims to change these numbers by developing a bioinspired composite scaffold that mimics the body’s natural healing processes to repair these muscle injuries. Using advanced imaging techniques and biomechanical simulations, researchers will design a scaffold to guide the regeneration of the muscle-tendon connection. The goal is to create a groundbreaking, long-lasting repair that can transform the treatment of childbirth injuries and significantly improve women’s health outcomes worldwide.

Dr. Elizabeth Krans received a 2-year $1,406,000 R61 grant from the NIH, titled “Impact of collaborative care for pregnant persons with opioid use disorder in low-resource obstetric settings.”
Context: Opioid use disorder (OUD) during pregnancy is a critical factor in maternal health risks in the U.S., as pregnant, postpartum, and parenting individuals (PPPP) with OUD facing unique barriers to initiating and sustaining treatment. Although medications for OUD (MOUD) can significantly reduce risks of overdose and preterm birth, many individuals struggle to access or remain in treatment. Compounding factors such as trauma, violence, and untreated mental health conditions increase the risk of relapse and overdose, especially during the postpartum period.
Project Aim: To address these challenges, collaborative care models (CCMs) have emerged as promising approaches that integrate care from healthcare providers, peers, and social services to support the comprehensive needs of PPPP with OUD. However, CCMs are typically found in large medical centers, limiting access for those in low-resource or rural settings.
This project will adapt a CCM for community-based, low-resource obstetric settings, focusing on areas with high rates of maternal opioid-related diagnoses, such as Northwest PA. This research hopes to provide essential insights for stakeholders and policymakers, with the goal of expanding effective, sustainable care models to underserved communities.

Dr. Sandra Cascio received a 1-year $215,000 supplement from the NIH, titled “The Role of Egfl6 in Tumor Immunity (Supplement).”
Context: Uterine serous carcinomas (USC) make up only 10% of endometrial cancers but contribute to nearly 40% of related deaths, highlighting a pressing need for better treatments. Immunotherapy shows promise across many cancer types, yet it has not been effective for USC.
Further investigation into the immune tumor microenvironment (TME) could help identify optimal immunotherapy strategies for USC, which is often marked by high levels of immune-suppressive cells. Research at MWRI has identified the protein EGFL6 as a potential target for improving USC treatments.
Project Aim: Through animal models, the team aims to study the EGFL6's impact on USC in combination with immunotherapy. Additionally, by analyzing EGFL6 expression and immune cell profiles in USC patients, with a focus on differences between Black and White women, the team hopes to advance precision therapies that improve survival in this aggressive cancer.

Dr. Miguel Brieño-Enriquez received a 1-year $232,000 R56 grant from the NIH, titled “Elucidating the role of the hyaluronan matrices on the establishment of ovarian reserve and aging.”
Context: Extracellular matrix plays pivotal roles in cell self-renewal, proliferation, fate, differentiation and maintenance in stem cells. Regulation of the ovarian reserve in mammals has been mostly focused on germ cell development; however, other ovarian elements, such as extracellular matrix, are poorly understood.
Project Aim: This project has an overall goal of understanding the mechanisms by which the extracellular matrices regulate the establishment of the ovarian reserve during development and how their maintenance can protect the ovary from aging.